A Guide to Telehealth for Patients and Providers

Before the spring of 2020, telehealth services were rarely used. Less than 1% of all insurance claims nationally in 2017 were for telehealth, according to FAIR Health, a nonprofit that analyzes insurance claims.
The technology was available, but the country had not bought in—that is, until the coronavirus pandemic. In April of 2020, FAIR Health’s Monthly Telehealth Regional Tracker reported an 8,335.5% year-over-year increase in volume of claim lines nationally, compared to 42.6% in January.
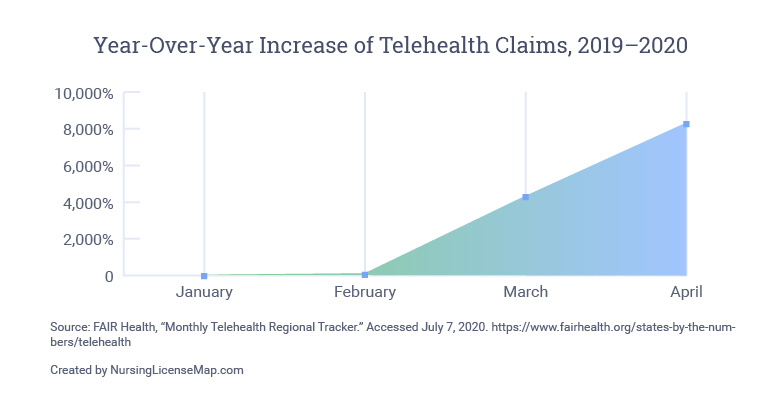
Go to tabular data showing the year-over-year increase of Telehealth claims from 2019 to 2020.
Matrix Medical Network, an organization of nurse practitioners providing at-home care and staffing mobile clinics, has conducted more than 50,000 telehealth visits since April. To keep up with demand, the company is hiring 200 to 300 new nurses a month, compared to the previous average of 100.
“It took a pandemic to wake up the nation to telehealth,
and now there’s no turning back.”
– Laura Jonsson, NP, senior vice president of clinical services at Matrix
As telehealth becomes more of a central part of the U.S. health care system, how can patients and providers prepare to make the most of interactions in this new reality?
The History of Telehealth and Nursing
For nurses, telehealth is not necessarily new. These health care professionals have long used available technologies to reach patients in need of care. Labor and delivery nurses both past and present field calls from pregnant women with possible labor signs. Nurses in the emergency department guide patients on whether to come in over the phone.
From an article on telehealth nursing in the journal Nursing: “Dating back to the 1970s, office nurses have communicated via telephone to discuss various healthcare issues with patients, including lab results, medication refill needs, and advice on how to manage minor illnesses at home.”
Telehealth nursing, or telenursing, describes nurses who care for patients through an audiovisual or audio-only connection, as indicated in the American Telemedicine Association’s 2019 position statement on telehealth nursing. The format has the potential to expand access to quality care, especially in remote and rural areas, but comes with its own set of barriers.
Telehealth refers to technology used to support health care and public health, encompassing remote clinical services, provider trainings, health administration and continuing medical education.
Telemedicine refers specifically to remote clinical services.
What Are the Benefits of Telemedicine?
Better Access to Care
Telehealth can begin to address some of the inequity in health care by removing the need for transportation.
Improved Frequency
Patients may be able to receive more regular access to care. In remote and rural areas, seeing a provider for routine care may involve a long, arduous drive that can be difficult and stressful, especially for older patients.
Shorter Wait Time
In the United States, patients have to wait an average of 24.1 days for a new physician appointment. In some clinics, a virtual visit may be more readily available.
Safer for Everyone
Having a virtual appointment during the coronavirus pandemic means people can avoid exposure to other patients as well as providers, who may come into contact with COVID-19 in daily rounds.
Comfort of Home
For patients, a clinical environment can feel cold and sterile. Seeing a provider from the comfort of home may help them feel more relaxed.
Fewer Distractions
In a clinic, providers often have many demands on their time, and appointments can feel rushed. In a telehealth visit, they may have more attention to give patients.
Still, telehealth presents its own challenges. For an audiovisual connection (the ideal setup), patients need reliable broadband connectivity and a device with a web camera or a smartphone with a data plan. Even an audio-only phone call with a provider may require extra minutes on a patient’s wireless plan. Each of these factors makes telehealth less accessible to individuals with lower incomes and those in rural or remote areas—one in four rural residents say high-speed internet access is a major problem in their communities.
How Does Telemedicine Work?
With telemedicine now more widely available, patients can schedule an appointment with their regular provider for continuity of care, or some insurance plans offer a telemedicine service that connects patients with a provider of their choice for a one-off visit.
Medicare places patient-facing telemedicine services into three categories:
E-visits:
Patient and provider communicate through an online patient portal without face-to-face interaction.
Telehealth visits:
Patient and provider communicate using a telecommunication system, such as an online video platform accessed through a computer, smartphone or tablet.
Virtual check-ins:
Patient and provider check in briefly via the phone or another device to decide if further services are necessary.
Provider-facing telehealth options include store-and-forward imaging and remote patient monitoring, both of which use technology to collect patients’ data remotely and send the information electronically to the provider for evaluation.
However, not all visits are appropriate for a virtual format. Lana Adzhigirey, RN, MN, CPHQ, recommends only offering telehealth to patients for whom a physical visit and a virtual visit would be of equivalent quality. Adzhigirey is the chair of the ATA Telehealth Nursing Special Interest Group.
“In those cases that we do not have enough evidence—for example, belly pain, any kind of abdominal pain is more difficult to assess virtually—we are more likely to make an in-person appointment,” she said.
Telehealth is typically not appropriate for serious or life-threatening conditions, including seizure, chest pain, head injury and difficulty breathing. The Centers for Disease Control and Prevention says telehealth services are best for these instances:
- Screening for COVID-19 symptoms
- Low-risk urgent care for non-COVID-19 conditions
- Primary and specialist care for chronic illness and mental health conditions
- Medication management
- Physical and occupational therapy
- Follow-up care after hospitalization
- Advance care planning and counseling
- Non-emergent care to residents in long-term care facilities

Telehealth Resources for Patients
What Can Patients Expect in a Telemedicine Appointment?
Expect bumps as you learn together.
Many providers are new to telemedicine, and they may feel out of their element. “They’re not able to do what is so natural to them, and that is to touch and assess patients physically,” said Adzhigirey. Try to be flexible when mistakes happen.
Your role may be more active.
Providers are now relying on the patient to communicate the physical indicators that they would typically observe and measure themselves at an in-person appointment. For the patient, this can even be empowering. “It gives an opportunity for patients to be very much more active in that interaction,” said Adzhigirey. Be prepared to use words and visuals to thoroughly describe your concerns.
Consider how involved you want to be.
You may be asked to take your own vital signs if the equipment is available. The provider may walk you through a physical exam. For example, Carl Marci, MD, chief medical officer of Ready, said an OB-GYN colleague “coaches the patient, and the patient pushes her own belly at different places.” If these requests make you uncomfortable, talk with your provider.
How Can Patients Prepare for a Telemedicine Appointment?
Write down descriptions of your concerns in advance.
Remember that the provider is depending more than ever on your words to understand your health status and your needs. Preparing your thoughts ahead of time can help you clarify your concerns.
Refresh your memory on health-related terms.
If needed, take a few minutes to review any medical terminology relevant to your care, especially for any chronic illnesses. Below, find links to glossaries of common terms related to some of the top chronic illnesses in the United States.
Know your medications.
Bring any medication containers or a list of their names and dosages to the virtual visit. Medication names can be complicated, so be prepared to spell them or sound them out.
Make a list of your health history and past surgeries.
This is always important, but it’s especially necessary to make sure new providers understand your health history. “That drives a lot of the decision-making and identifying what the right treatment is,” said Jonsson. Putting it to paper can prevent forgetfulness.
Get ready for any physical exams.
If your visit will involve a physical exam, prepare your environment and your body. For example, a patient with diabetes may need a lower extremities exam. “Have shorts on if you need us to look at the legs, or have your shoes and socks off if there’s something with the feet,” said Jonsson.
Get a callback number.
Before the visit officially starts, ask for a callback number. If you lose the connection or the audiovisual technology does not work, you can shift to a phone call.
Telehealth Resources for Providers
How Can Providers Prepare for a Telemedicine Appointment?
Reframe the situation for yourself.
Adzhigirey encourages providers to consider telehealth technology as simply another tool that works for patients at that time, instead of as a hindrance. “Patients still need our care and need our partnership,” she said. “It’s our job to meet people where they are.”
Make the technology a permanent part of your skill set.
Because telehealth is likely to stay even after the pandemic, using the technology will become an essential skill for providers. Like any other skill, it will require training and intentional practice to become proficient.
Practice telepresence etiquette.
Establishing trust with patients from the moment you connect is key. “Patients need to know that you are a professional and that you are located in a space where they can have a private conversation,” said Adzhigirey. A few tips include:
- Look at the camera rather than the screen.
- Make sure both you and your background look professional.
- Tell the patient when you look at your notes (e.g., “I’m going to look away for a moment to capture what you’re saying”).
Give the patient time to talk.
In a virtual visit, the provider may have a harder time picking up on cues that the patient has more to say. Take extra care to ensure they are heard. “You want to be careful not to speak over them, and that’s harder through video, especially when the connection may not be perfect,” said Marci. Keep checking to make sure you both are on the same page.
Recommendations for Protecting Patients’ Privacy
Get verbal consent.
HIPAA law requires providers to activate all available encryption and privacy features when using videoconferencing applications. Before starting the patient visit, explain that your service is two-way encrypted and ask for their verbal consent to begin.
Turn off recording.
For videoconference platforms, do not record virtual interactions with patients. Administrators may consider turning off the function at the systems level.
Check your windows before screen-sharing.
If you choose to share your screen with a patient, make sure that files for any other patients are closed or hidden.
For patients and providers, getting comfortable with telemedicine will take time, and there may be a learning curve. But the benefits of improved access and better patient safety are clear.
“Even as a provider myself, I was a little nervous for my first [telehealth] visit,” said Jonsson. “But it went flawlessly.”
Year-Over-Year Increase of Telehealth Claims, 2019–2020
Month | Year-Over-Year Increase (%) |
January | 42.6 |
February | 121.3 |
March | 4,346.9 |
April | 8,335.5 |
Source: FAIR Health, “Monthly Telehealth Regional Tracker.” Accessed July 7, 2020. https://www.fairhealth.org/states-by-the-numbers/telehealth
Created by NursingLicenseMap.com
< Treating Student-Athletes With Sports Concussions
> Eating Disorder Recovery Is Possible, Even During a Crisis: Activities and Affirmations