Treating Student-Athletes With Sports Concussions

A school nurse’s work is more than simply assessing scrapes and taking temperatures. “The school setting for a nurse involves a little emergency nursing, a little intensive care knowledge,” said Cameron Traut, MS, BSN, RN, NCSN, PEL-IL — as well as community health, infectious disease, and pediatric and adolescent medicine.
Transitioning to school nursing at Libertyville High School in Libertyville, Illinois, Traut found her experience nursing in the pediatric intensive care unit served her particularly well for treating one specific injury prominent in youth athletics: sports-related concussions.
Unlike a broken leg or torn ligament, a concussion can permanently affect a student’s ability to learn and function academically. The long-term cost may be much higher than just a missed season.
At the intersection of healthcare and education, school nurses are poised to promote student athletes’ concussion recovery through treatment, patient education and leadership. What would they want students and their families, educators and coaches to know?
What Are Concussion Signs and Symptoms?
Concussion symptoms may be obvious and occur soon after the head injury, such as losing consciousness or vomiting. However, they may be subtle and appear over time.
The majority of sports-related concussions do not involve losing consciousness, according to the 2016 Zurich Consensus on Concussions (PDF, 608KB). This reality can make them tough to spot. The student may “just not feel right,” said Traut.
The student may seem out of sorts to their family, friends, teammates and coaches. “They’re zoning out, spacing out. They just don’t appear like they’re quite right,” she said.
Educators may notice changes in the classroom. Concepts mastered before the injury may suddenly become more challenging.
“Up until the injury, they may have been really good at math and could figure these things out quickly,” said Traut. “After the concussion and during recovery, it’s really difficult for them.”
CONCUSSION SIGNS OBSERVED
- Lack of recall
- Dazed or stunned appearance
- Forgetfulness or confusion
- Clumsiness
- Changes in behavior, mood or personality
- Slow response to questions
CONCUSSION SYMPTOMS REPORTED
- Headache or pressure in head
- Nausea or vomiting
- Dizziness or trouble balancing
- Blurry vision
- Sensitivity to light or noise
- Difficulty concentrating or remembering
- Low mood or just “not feeling right”
Who Is Involved in Concussion Treatment?
Among sports medicine providers, concussions are considered one of the most complex injuries to manage, as stated in the Zurich Consensus. Treating concussed children and adolescents may be especially delicate, as their brains are still developing.
A student-athlete’s concussion team includes healthcare professionals and their support system at home, in school and on the field.
School Nurse: Helps manage the student-athlete’s care and recovery, coordinating their care providers, athletics staff and educators. As needed, the school nurse provides daily assessments of the student’s status and helps them understand and communicate their symptoms, thoughts and feelings. The school nurse’s role differs by state legislation, school policy, severity of the concussion and the student’s needs and preferences.
Specialized Care Provider(s): Monitors the student-athlete’s progress and develops the protocol for returning to activity. The community care provider may be an advanced practice nurse practitioner, pediatrician, concussion specialist, neurologist, sports medicine physician or physician’s assistant. The school nurse helps enact their treatment plan.
Mental Health Counselor, School Counselor or Social Worker: Supports the student’s emotional health in the aftermath of the injury. Concussion recovery sometimes involves major life adjustments, and a mental health professional can help them cope.
School Educators: Work with the school nurse to adapt schoolwork as needed to support the student’s academic growth and concussion recovery simultaneously.
School Athletics Staff: Help manage the student-athlete’s safe return to activity and play, working with the school nurse to set the return-to-play protocol into motion.
Family and Friends: Can offer stability during a potentially scary or frustrating season. School nurses support parents or guardians in particular by providing reassurance and counsel.
Read a full transcript of the infographic Sports-Related Concussions by the Numbers.
Concussion Helmets: How Head Protection Has Changed With Healthcare Advances
Football players experience some of the highest incidence rates of concussions among all sports. Protecting them has become a public health priority. The evolution of players’ head protection reflects the health field’s developing understanding of concussions and athletes’ long-term mental health.
Read a full transcript of the infographic One Hundred Years of Helmet Innovations.
Where to Learn More About Sports Concussions and Recovery
CDC’s HEADS UP, The Centers for Disease Control and Prevention: Provides guidance written specifically for parents, schools and healthcare providers on spotting, treating and preventing concussions, as well as information on sports concussion policies and laws.
Concussion, Mayo Clinic: Offers an overview of concussion causes and symptoms and addresses a common question about concussions: when to seek treatment.
Concussions – The Role of the School Nurse, The National Association of School Nurses: Describes the organization’s official statement on the school nurse’s role in referring students for concussion treatment, supporting their recovery and managing their return to activity, play and class.
Fact Sheet for School Nurses, The Centers for Disease Control and Prevention: Prepares school nurses to recognize and respond to concussions in the moment and outlines how to monitor students’ recovery long term. This handout also offers five tips on how to prevent concussions in sports at school.
Sports Concussions (For Teens), TeensHealth: Defines sports concussions in an accessible way for older children and adolescents.
Youth Football Helmet Ratings, Virginia Tech: Posts ratings of youth football helmets’ ability to reduce linear and rotational acceleration — in other words, their ability to protect players from sustaining a head injury when collisions happen.
Legal Disclaimer: Please note that this article is for informational purposes only. Individuals should consult their health care provider before following any of the information provided.
The following section includes real text from the graphics in the post.
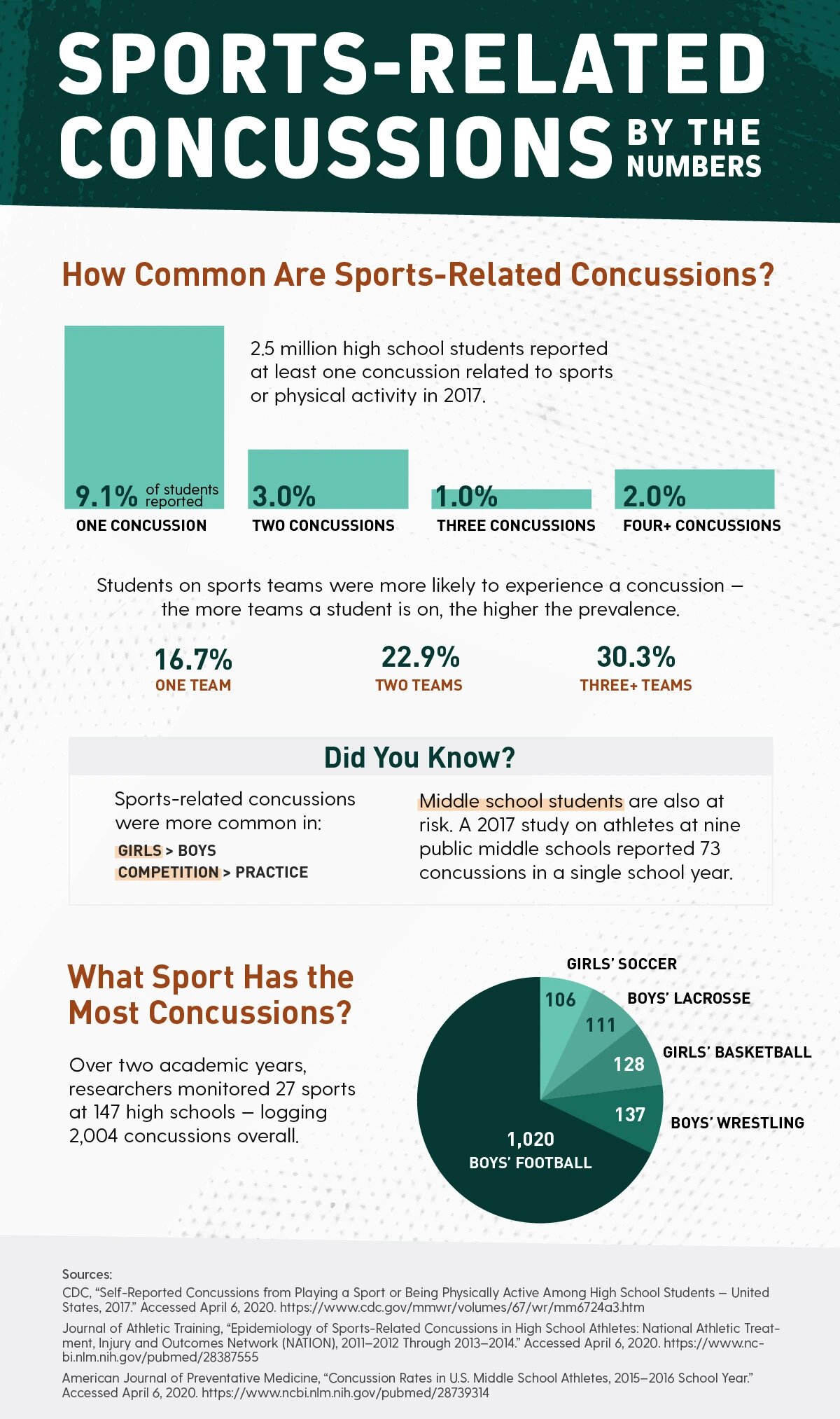
Sports-Related Concussions — By the Numbers
How Common Are Sports-Related Concussions?
2.5 million high school students reported at least one concussion related to sports or physical activity in 2017.
- 9.1% of students reported one concussion
- 3.0% of students reported two concussions
- 1.0% of students reported three concussions
- 2.0% of students reported four or more concussions
Students on sports teams were more likely to experience a concussion — the more teams, the higher the prevalence.
- If on one team there was a 16.7% chance of concussion
- If on two teams there was a 22.9% chance of concussion
- If on three or more teams there was 30.3% chance of concussion
What Sport Has the Most Concussions?
Concussion rates vary by sport. Over two academic years, researchers monitored 27 sports at 147 high schools — logging 2,004 concussions overall, including:
- Boys’ football logged 1,020 concussions
- Boys’ wrestling logged 137 concussions
- Girls’ basketball logged 128 concussions
- Boys’ lacrosse logged 111 concussions
- Girls’ soccer logged 106 concussions
Did You Know?
Sports-related concussions were more common in:
- Girls than Boys
- Competition than Practice
Middle school students are also at risk. A 2017 study on athletes at nine public middle schools reported 73 concussions in a single school year.
Sources:
- CDC, “Self-Reported Concussions from Playing a Sport or Being Physically Active Among High School Students — United States, 2017.” Accessed April 6, 2020.
- Journal of Athletic Training, “Epidemiology of Sports-Related Concussions in High School Athletes: National Athletic Treatment, Injury and Outcomes Network (NATION), 2011–2012 Through 2013–2014.” Accessed April 6, 2020.
- American Journal of Preventative Medicine, “Concussion Rates in U.S. Middle School Athletes, 2015–2016 School Year.” Accessed April 6, 2020.
Back to Sports-Related Concussions — By the Numbers graphic
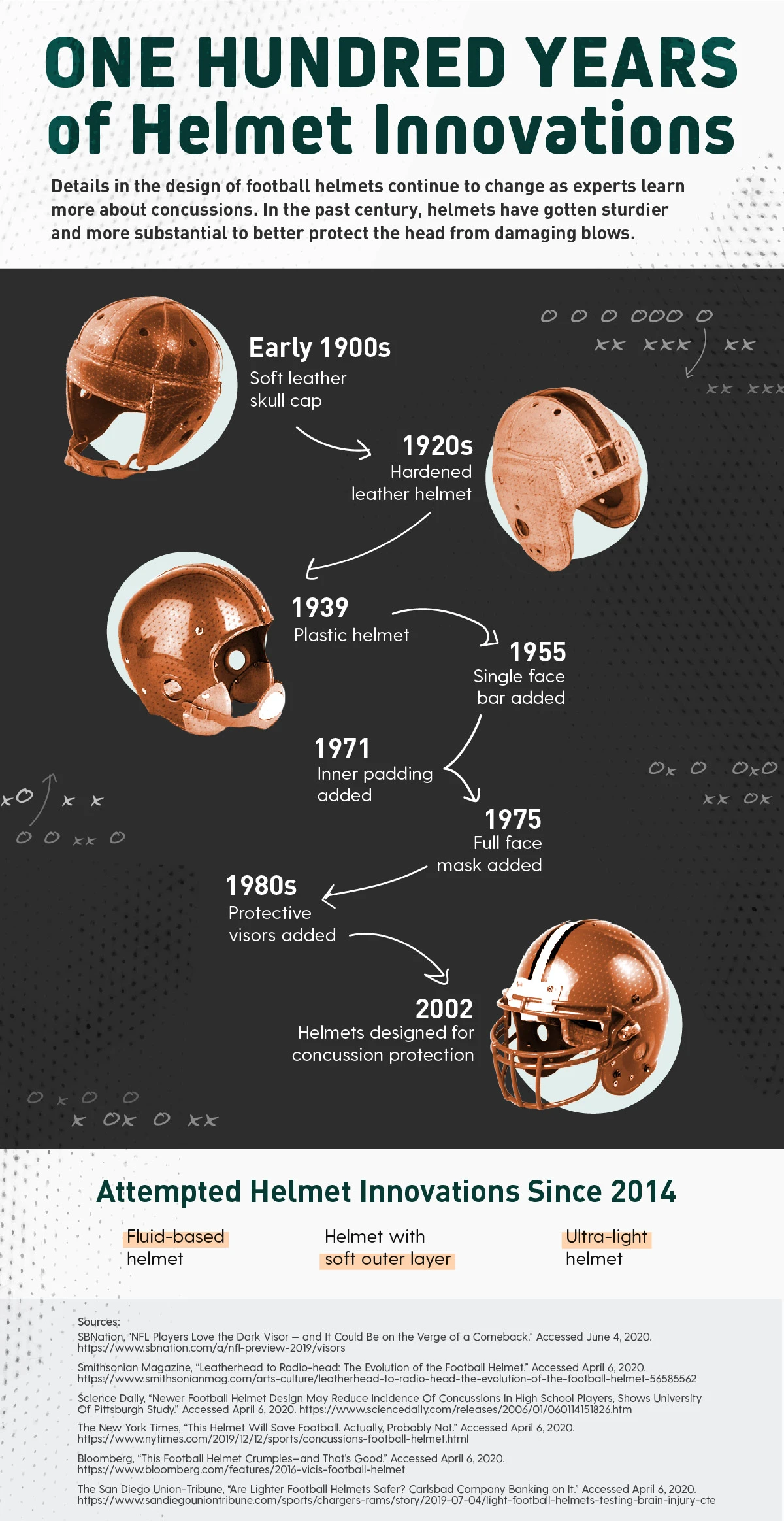
One Hundred Years of Helmet Innovations
Details in the design of football helmets continue to change as experts learn more about concussions sustained by players. In the past century, helmets have gotten harder and more substantial to better protect the head from damaging blows.
- Early 1900s – Soft leather skull cap
- 1920s – Hardened leather helmet
- 1939 – Plastic helmet
- 1955 – Helmets with a single face bar
- 1971 – Helmets with inner padding
- 1975 – Helmets with a full face mask
- 1980s – Helmets with protective visors
- 2002 – Helmets designed for concussion protection
Attempted Helmet Innovations Since 2014
- Fluid-based helmet
- Helmet with soft outer layer
- Ultra-light helmet
Sources:
- SBNation, “NFL Players Love the Dark Visor — and It Could Be on the Verge of a Comeback.” Accessed June 4, 2020.
- Smithsonian Magazine, “Leatherhead to Radio-head: The Evolution of the Football Helmet.” Accessed April 6, 2020.
- Science Daily, “Newer Football Helmet Design May Reduce Incidence Of Concussions In High School Players, Shows University Of Pittsburgh Study.” Accessed April 6, 2020.
- The New York Times, “This Helmet Will Save Football. Actually, Probably Not.” Accessed April 6, 2020.
- Bloomberg, “This Football Helmet Crumples—and That’s Good.” Accessed April 6, 2020.
- The San Diego Union-Tribune, “Are Lighter Football Helmets Safer? Carlsbad Company Banking on It.” Accessed April 6, 2020.
Back to One Hundred Years of Helmet Innovations graphic.

