A Nurse’s Toolbox for Parenting a Child with Chronic Pain

Research estimates that up to one-third of children and adolescents experience some form of chronic pain, which can interrupt their schooling, extracurricular activities and other parts of daily life. Although it may be difficult for children to work through pain to maintain their routines, parents and educators can help teach young children and teens coping mechanisms that they can draw on to manage their pain, stay in school and remain engaged with their social lives.
“The main thing is making a team effort — whether it is a hospital collaborative team that’s working with a child inpatient, or whether it is a family or a school system, the child can’t do this on its own,” said pediatric nurse practitioner and nurse educator Beth Fisher, PNP, APRN, CPNP, CPON. “It’s got to be people that are in their corner that are going to want to work with them, but the child has to have expectations too.”
Read on to learn about pediatric chronic pain causes and activities that can be used to manage the pain.
Types of Chronic Pain Disorders in Children
The three most common categories of chronic pain disorders in pediatrics are:
Primary headaches
Centrally mediated abdominal pain syndromes
Chronic musculoskeletal and joint pain
Pediatric Chronic Pain Causes
Common pediatric chronic pain causes and different chronic pain conditions in children include:
- Amplified musculoskeletal pain (AMPS)
- Chronic or recurrent abdominal pain
- Chronic fatigue syndrome
- Chronic headache
- Complex regional pain syndrome (CRPS)
- Fibromyalgia
- Musculoskeletal pain, including back pain
- Hypermobility syndromes
- Myofascial pain
- Nerve injuries
- Neuropathic pain
- Pain secondary to acute or chronic illness, or related to injuries or surgeries
- Postural orthostatic tachycardia syndrome
- Sickle cell anemia
- Somatic symptom disorders
What To Do When You Find Out Your Child Is Experiencing Chronic Pain
Managing children’s chronic pain begins with acknowledging their pain.
“Pain is what the person says it is, and if we don’t show them that we believe their pain is real and treat that pain, we’re going to lose them from the very beginning,” Fisher said. “So, I say treat the pain they have and let’s work on what’s behind the source. Is it real? Is it imagined? Is it used as manipulation? We’ll get to that, but we’ve got to show them that we trust them, that we are hearing what they’re saying.”
Once parents establish that their child is dealing with chronic pain, it is important to give them tools to work through their pain to maintain or return to a routine. A parent’s response has to be different than if their child is experiencing an acute illness, said licensed clinical psychologist Jody Thomas, who founded the Meg Foundation, an organization that works to empower families to prevent and relieve pain.
“If we can offer opportunities to cope during the day, we can extend their ability to be at school successfully.”
–Jody Thomas, licensed clinical psychologist
“Our typical parenting instinct is often to treat it kind of like if our kid has the flu, and we put them on the couch and we bring them soup and let them watch TV,” Thomas said. “That’s really fantastic if they have the flu for a few days. It becomes a very destructive dynamic for chronic pain because it reinforces that role.”
Instead, parents should encourage children to function through pain, set expectations and give them strategies to lessen pain as they continue with their routines and activities.
“One of the huge, and to be frank, ridiculously unfair truths about chronic pain recovery is we will say function will come back before pain relief,” Thomas said. “We can’t wait to function until the pain goes away because we’ll be waiting indefinitely. We will become less functional. We will become atrophied, and we will have a lot more pain issues.”
How Can I Help My Child With Chronic Pain?
Parents and caregivers can use a combination of physical, psychological and pharmacological coping mechanisms and treatments to help children through their pain.
One of the phrases Thomas has used with pediatric pain patients to help them regain control of their pain and their lives is, “This is not your fault, but it is your responsibility.”
“I’m not saying that you did this or are trying to do this, but I am saying you’re the only one who can fix it,” Thomas said. “That’s a hard message. Our role as providers, and our role as parents and as people are to support that coping.”
These strategies may help parents assist their children
in managing chronic pain.
- Teach children to tell teachers and other adults how they are feeling.
- Maintain routines in school, sleep and exercise, balancing periods of physical activity with rest.
- Give students credit for attending school and other activities, and reward them with simple and inexpensive prizes, such as earning extra screen time.
- Create group rewards that involve family members and/or friends to celebrate children for engaging in activities that will help improve their pain, such as doing physical therapy or sticking to a medication schedule.
- Track children’s progress visually using a phone app, sticker chart or other visual aid.
- For special events and other occasions, create a game plan for how to handle painful episodes that may arise.
- Don’t focus on the child’s pain or ask your child if they are hurting; let them bring it up instead.
- Avoid centering your child’s pain as part of their self-image.
- Be aware how you respond to your own pain.
Activities for Chronic Pain Relief
In addition to maintaining a pain medication regimen, other activities can help mitigate chronic pain. Fisher suggests finding activities that a child is interested in, such as puzzling, coloring or listening to their favorite music, to tone down the pain.
“I can’t promise them we’ll get rid of pain, whether it’s chronic or acute, but what I do want to help them do is think about their response to pain and what can we do to control our response to pain,” Fisher said. “Learning things like mind-body activities, like deep breathing, focus activities — that allows us a little more control over who’s in the driver’s seat: you or the pain.”
Examples of nonpharmacological interventions to soothe children with chronic pain include:
- Art therapy
- Biofeedback (e.g., massage, acupuncture, acupressure)
- Guided imagery and meditation
- Hypnosis and self-hypnosis
- Passive and active distraction (e.g., music, coloring, puzzling)
- Physical and occupational therapy
- Progressive muscle relaxation
- Therapeutic recreation
“The reason those things are so important is not only that they are effective, but they also put the power in the hands of the child,” Thomas said.
Activities for Chronic Pain Management
Children may use some of the techniques below to soothe themselves when they are in pain and help maintain their normal routines.

- Purse your lips like you’re blowing out a candle and slowly exhale all the air from your lungs until you have released all the air from your chest and belly. Exhale for about five seconds.
- Feel your shoulders relax, your neck relax, your muscles loosen and your body become comfortable. Pause for a moment and hold on to this peaceful state.
- Seal your lips and draw a breath in through your nose for a count of five seconds, filling your chest and belly with air. You can place a hand on your belly to notice your belly inflating with air.
- Keep your muscles calm and relaxed.
- Repeat these slow inhales and exhales for four to five rounds of breath.

- Tighten and relax your muscles from your head to your toes.
- Begin with your scalp and forehead, tighten the muscles and release.
- Tighten and release the small muscles in your face — your cheeks, lips, jaw, etc.
- Tighten and relax your neck muscles.
- Keep moving down the body — through your chest, arms, torso and legs — tightening and relaxing each muscle group until you reach your toes.
How to Manage Chronic Pain in School
Managing chronic pain can be isolating for children, even if they are able to remain in school.
“A lot of folks at schools, hospitals, clinics, doctors, nurses — they sometimes think a child is acting a lot more sleepy and not participating because they are just being uncooperative and not really in pain. And sleep and fatigue and things are just a coping mechanism for pain,” Fisher said. “That leads to isolation where they’re not really wanting to participate or be around their peers.”
Parents and caregivers should work with school staff and faculty to create an action plan that can help students work through their pain while remaining in school.
“We can’t wait to function until the pain goes away because we’ll be waiting indefinitely. We will become less functional. We will become atrophied, and we will have a lot more pain issues.”
–Jody Thomas, licensed clinical psychologist
“If we can offer opportunities to cope during the day, we can extend their ability to be at school successfully,” Thomas said.
That could mean not placing limits on bathroom breaks for students with abdominal pain, or creating designated break rooms for students to go when they need a quiet place to use their coping skills.
“One thing that keeps kids out of school when they’re dealing with chronic pain is parents knowing that they’re going to get called at the drop of a hat for everything, and if they’re trying to work, that’s just not going to work,” Fisher said. “Having a plan like that in place gives the parents confidence that they know that the school knows how to take care of their child’s pain.”
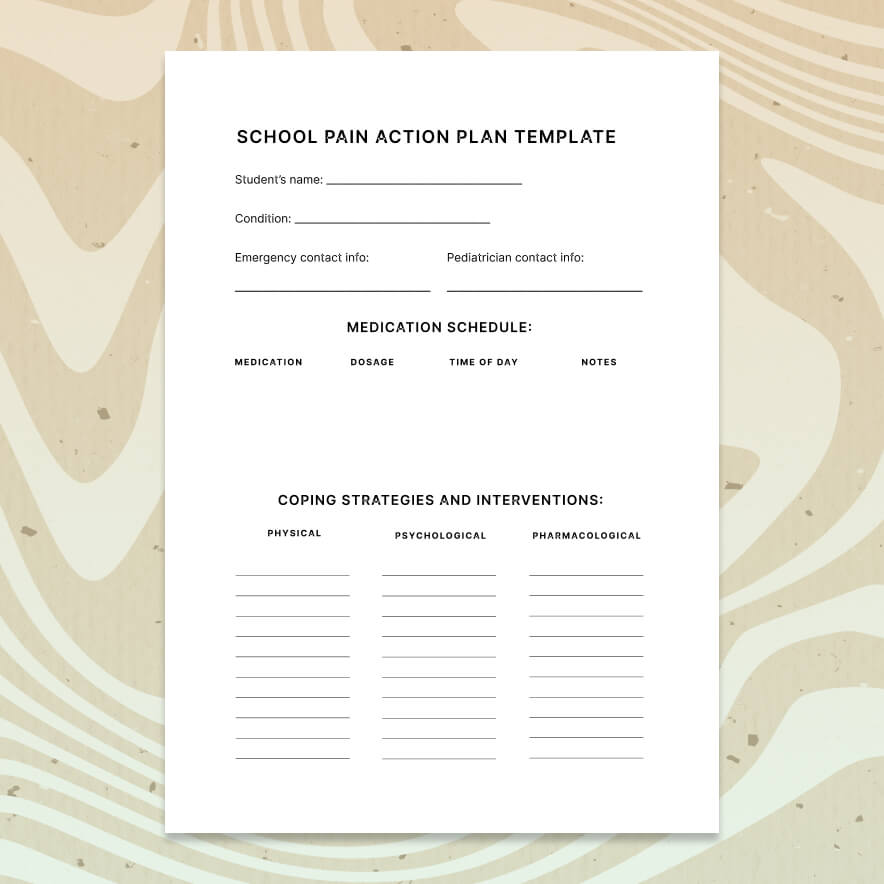
These steps can help families create an action plan to keep children with chronic pain in school.
1
Create a team. Identify a point person in the school — a teacher, guidance counselor or school nurse — for the student to go to when they are experiencing pain.
2
Identify coping mechanisms. Identify strategies the student can use to work through pain at different pain levels. These could include strategies such as taking short breaks for deep breathing in a quiet place, taking medication, or engaging in distractions such as listening to music.
3
Make a pain action plan. Create a plan that outlines how a student can handle pain when it reaches different levels (see the downloadable template below for building a basic pain action plan), including appropriate places for the student to take breaks throughout the day. If your child qualifies, consider working with the child’s school to seek accommodations and create a formal individualized education program (IEP).
4
Hold a team meeting. Meet with stakeholders to get everyone on the same page, especially if the student is returning to school after an extended absence. Involve the student in the meeting and decision-making if age appropriate, and set expectations for staying in school.
5
Check in with the student throughout the school year. “A lot of times once we see a child labeled with something and they have a treatment plan and they seem to look OK on the outside, we forget that they may not really be OK,” Fisher said. “You’ve got to be able to work as a team together and not make assumptions.”
Additional Chronic Pain Resources
Please note that this article is for informational purposes only. Individuals should consult their health care provider before following any of the information provided.